By Alan Budenz, M.S., D.D.S., M.B.A
From the Spring 2023 Journal of the Colorado Dental Association
Introduction
The Gow-Gates mandibular division nerve block injection technique is considered by many researchers and dental practitioners to be the most successful, consistent, and efficient method for obtaining mandibular quadrant anesthesia for dental procedures1-3. The Gow-Gates technique also has the lowest incidence of reported side-effects or complications. Yet many practitioners find the technique difficult to understand and to master, primarily due to the use of extra-oral landmarks.
The extra-oral landmark modifications for the Gow-Gates injection technique that are introduced in this article have been taught at the University of the Pacific, Arthur A. Dugoni School of Dentistry for several years, and have been found to be easily learned and used by dental students and by practicing dentists and dental hygienists attending hands-on technique training courses. These modifications build upon both the original description of the technique by Dr. George Gow-Gates4 and upon later modified descriptions by other authors but incorporate what we at Pacific Dugoni have found to be a simpler method for determining the correct target point and the proper angulation of the syringe in the medial-lateral orientation.

Figure 1 Lateral Angle Clinical Slide
Modified Extra-oral Landmarks for the Gow-Gates Injection Technique
Step 1: Our modified technique begins by observing and extra-orally palpating the head of the condyle as the patient opens and closes their jaw. With jaw movement, the clinician can see the bulge of the cheek created by the head of the condyle during opening and closing and can feel the condyle as it slides anterior-posteriorly over the articular eminence of the temporal bone.
Step 2: After first palpating the bulging condylar head extra-orally, the clinician then slides their index finger inferiorly below the head of the condyle, and then posteriorly behind the neck of the condyle.
Step 3: With the finger kept in this position and the mouth wide open, the clinician next palpates the anterior border of the mandibular ramus intra-orally, either at or slightly above the depth of the coronoid notch.
Step 4: With the mucosa pulled taut anteriorly, the clinician then inserts the needle at the intra-oral penetration site and aims the needle directly toward their finger. We teach a penetration site at a level just below the distobuccal cusp of the maxillary second molar or just distal to this tooth. Because the extra-oral finger is held posterolateral to the targeted neck of the condyle, it is directly behind the injection target. As long as the needle is aimed directly toward the finger/condylar neck from the penetration site, failure to contact bone is unlikely. Alignment of the injection path with the extra- and intra-oral landmarks is easily assessed both when applying topical anesthetic before the injection and during the injection by simply “leaning back” from the oral cavity and visually checking that the needle pathway intra-orally is directed toward the fingertip behind the condylar neck extra-orally and correcting the needle angulation if necessary (Figure 1).
Note: The patient’s mouth must be fully open throughout all phases of the Gow-Gates injection. The condyle then assumes an anterior position over the articular eminence of the temporal bone that is immediately lateral to the trigeminal mandibular division nerve trunk as it emerges through the foramen ovale of the cranial base into the infratemporal fossa. The advantages of this modified approach are multiple.
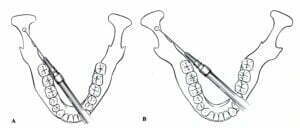
Figure 2 Lateral Angle Mandibles Jastak
- Familiar landmarks: With palpation of the anterior border of the mandibular ramus intra-orally and the posterior border of the ramus extra-orally, although at a higher level, the landmarks used are similar enough to the familiar conventional inferior alveolar regional nerve block landmarks that practitioners are immediately confident with them. With the clinician then aiming for their extra-oral finger directly behind the desired target, the condylar neck of the mandible, the injection pathway is more readily understood. Use of these familiar and definitive mandibular landmarks anteriorly and posteriorly also enables use of the same mind visualization skills that are used with the conventional inferior alveolar injection technique. However, instead of visualizing a “bisection” point for bony contact between the two landmarks, we are visualizing a path aimed directly at the posterior landmark. It is in large part because of this similarity of visualization skills that both inexperienced dental students and seasoned practitioners are able to more quickly master consistent success with this modified Gow-Gates injection technique. This is certainly a simpler visualization concept than the rather abstract visualization of the imaginary alpha and beta planes described by Dr. Gow-Gates and where they intersect. It is also our experience that palpation of the neck of the condyle relative to the anterior border of the ramus provides a more individual, and therefore more accurate, assessment of the degree of lateral flaring of the posterior ramus rather than relying on the soft tissue variability of the angulation of the tragus of the ear away from the face (Figure 2).
- High success rate: As with all variations of the Gow-Gates technique, the greatest advantage is the high success rate for anesthesia of all the sensory branches of the mandibular division of the trigeminal nerve with a single injection.
- Safety: The high success rate is coupled with a very low incidence of complications such as positive aspirations, hematoma, trismus, or nerve injury.
- Positive aspiration at the injection site is very low with the Gow-Gates technique with a reported incidence of less than 2%1,2,5,6. This is due to the needle passing through a region of relatively avascular loose fatty areolar tissue on its course to the anterolateral neck of the condyle7.
- The incidence of trismus is also extremely low due to the passage of the needle below the insertion of the inferior head of the lateral pterygoid muscle and medial to the position of the medial pterygoid muscle1,2,4,7.
- Nerve injuries, such as paresthesia, are rarely observed with the Gow-Gates technique. At the bony contact site, the needle is 10 to 20 mm lateral to V3 so direct contact with this large neurovascular bundle is avoided3,7.
Conclusion
This modified approach provides a reliable, and quickly learned, technique for the everyday clinician to use for successful mandibular division nerve block anesthesia because the landmarks are familiar and are determined individually for each patient.
References:
- Malamed SF. Handbook of local anesthesia. 5th St. Louis, Elsevier Mosby; 2004, Chapter 14: Techniques of Mandibular Anesthesia, pp. 227-242.
- Haas DA, Alternative mandibular nerve block techniques: A review of the Gow-Gates and Akinosi-Vazirani closed-mouth mandibular nerve block techniques, JADA, 142(9 suppl):85-125, 2011.
- Malamed SF, The Gow-Gates mandibular block: Evaluation after 4,275 cases. Oral Surg Oral Med Oral Path, 51(5):463-467, 1981.
- Gow-Gates GAE, Mandibular conduction anesthesia: A new technique using extraoral landmarks. Oral Surg Oral Med Oral Pathol, 36(3):321-328, 1973.
- Clark S, Reader A, Beck M, Meyers W, Anesthetic efficacy of the mylohyoid nerve block and combination inferior alveolar nerve block/mylohyoid nerve block. Oral Sur Oral Med Oral Path, 87(5):557-63, 1999.
- Meechan JG, Practical Dental Local Anesthesia. London, Quintessence Publishing Co. Ltd.; 2002, pp. 65-66.
- Gow-Gates GAE, Watson J, The Gow-Gates mandibular block: Further understanding. Prog. 25(6): 183-189, 1977.
- Hung P-C, Chang H-H, Yang P-J, Kuo Y-S, Lan W-H, Lin C-P, Comparison of the Gow-Gates mandibular block and inferior alveolar nerve block using a standardized protocol, J Formos Med Assoc 105(2): 139-146, 2006.
Alan W. Budenz, M.S., D.D.S., M.B.A., is an Emeritus Professor in the Department of Biomedical Sciences and Department of Diagnostic Sciences at the University of the Pacific, Arthur A. Dugoni School of Dentistry. Contact him at 415-929-6574 or abudenz@pacific.edu.
| Dr. Alan Budenz will be a featured CE speaker at the CDA Annual Session on Saturday, June 10 at the Viewline Resort Snowmass. Register for his courses and join your colleagues for a family-friendly weekend at the CDA Annual Session: cdaonline.org/annualsession |


