From the Journal of the Colorado Dental Association Winter 2025
By Boyd Tomasetti, D.M.D.; Jonathon Fergus, D.D.S.; Akshay Shah, D.D.S; and Sara Anderson, D.D.S., M.D.
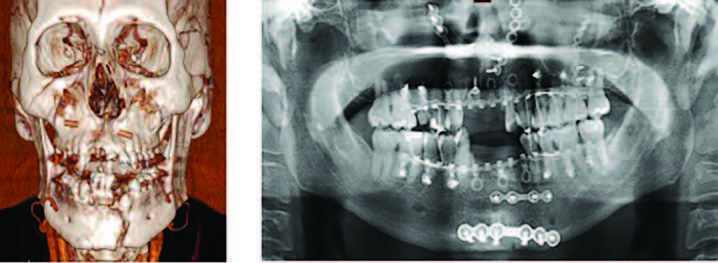
1a: 3-Dimensional reconstruction of CT facial bones showing facial fractures at time of presentation. 1b: Panorex radiograph obtained post-operatively showing reduction and fixation of facial fractures.
Introduction
The use of e-scooters has become an increasingly popular form of transportation in the Denver metro area. Their low cost, easy procurement and convenience, particularly in more congested downtown areas have made them an increasingly attractive mode of transportation for both commuters and those looking for a late-night ride. Unfortunately, this has also come with an ever-increasing number of crashes resulting in facial and dental injuries. Emergency departments and private practitioners across Colorado’s metro areas are now dealing with the ramifications of these accidents.
As one of the busiest Level 1 trauma centers in Colorado, Denver Health is seeing a myriad of injuries involving the face and teeth. The Oral and Maxillofacial Surgery (OMS) Department is the primary treatment provider for these crashes. Most of the crashes are single user crashes but pedestrian, auto and other vehicles were also involved. Injuries range from lacerations to pan-facial fractures and often involve dental trauma. Causative factors included lack of experience in e-scooter use coupled with behavioral issues — alcohol being a prime factor. Additionally, many patients were first-time e-scooter riders and were unfamiliar with e-scooter handling and varied road conditions.
Materials and Methods
The OMS service is on call for facial trauma at Denver Health two of every three days. The most common injuries the OMS service is called to evaluate and treat are fractures of the facial bones and complex facial lacerations. The General Practice Residency (GPR) dental residents are on call for dental trauma 24 hours per day, 365 days per year. Dental residents are typically consulted for Ellis class III and IV fractures as well as displaced teeth and associated alveolar housing fractures.
Each OMS/facial trauma and dental consult from July 1, 2023, to Aug. 15, 2024, was reviewed and sorted by chief complaint and principal diagnosis for emergency department visit. There were 1,096 facial trauma consults and 520 dental consults during this time. Of these, 121 patients met inclusion criteria of documented chief complaint or principal diagnosis of e-scooter accident. Ninety-seven patients required evaluation by OMS, and 40 patients required evaluation by dental residents. Twenty-two patients required evaluation by both the OMS and dental teams, indicating that there were both facial and dental injuries identified. Each patient’s electronic health record was reviewed to classify injury patterns, identify whether alcohol and/or drugs were a factor in the accident, and determine if the patient required surgery as a result of the injuries. Facial fractures were classified by regions. The upper facial third includes fractures of the frontal bone. The mid-face includes fractures of the zygomaticomaxillary complex, orbit, maxilla and nasal bones. The lower facial third includes fractures of the mandible. Dental injuries included fractured teeth, displaced and avulsed teeth, and alveolar housing fractures. Lacerations that required repair by OMS, dental, or the emergency department were documented as well.
Results
Facial fractures were the most common injury in patients evaluated. Ninety patients in total were found to have facial fractures, with 15 fractures of the upper facial third, 55 of the mid-face, and 20 fractures of the lower facial third. Eight patients had fractures that involved multiple facial thirds. Thirty of the patients required surgery. Of these, 20 patients required an open reduction and internal fixation (ORIF) of the fractures. Four patients required an ORIF plus application of arch bars with maxillomandibular fixation (MMF). Six patients with fractures of the mandibular condyle and/or condylar process had closed reduction with MMF.
Dental injuries were identified in 43 patients. These patients typically required reduction of displaced teeth or alveolar fractures with placement of a resin-bonded splint. Some patients also received direct pulp cap with calcium hydroxide, glass ionomer and/or flowable composite for Ellis class III or IV fractures. Seventeen of the patients with dental injuries were also found to have facial fractures.
The mechanism of injury from an e-scooter crash frequently results in facial lacerations. Forty-six patients’ dental or facial injuries were accompanied by a complex facial laceration that required suture repair. The most common lacerations involved the peri-oral regions and often had full-thickness, intraoral and extraoral components.
Lastly, through review of provider notes, we noted whether drugs or alcohol were factors in the accidents. Eighty out of the 119 patients reviewed were noted to have some level of alcohol intoxication at the time of their accident. Twenty-one patients were negative for alcohol intoxication, and it is unclear if alcohol played a role for 18 of the patients. Two patients reported marijuana use prior to their accident. Unlike alcohol, marijuana use is not robustly screened for and reported in trauma cases so it is undetermined if more patients were under the influence of marijuana.
Discussion
The findings of this limited review of data support feelings from both OMS and dental providers that e-scooter crashes cause a significant amount of facial and dentoalveolar trauma in the Denver metro area. It is worth noting that the inclusion criteria for thorough chart review were only patients with documented chief complaint or principal diagnosis of an e-scooter accident. The data reported in this study certainly underreports the true volume of e-scooter related injuries, since some patients end up with other diagnoses or chief complaints attached to their records (some examples being “facial pain,” “dental trauma,” “fall,” “head injury,” etc.). Even with this taken into consideration, the e-scooter accidents reviewed accounted for approximately 9% of total consults for OMS residents and approximately 8% of total consults for GPR dental residents.
The OMS and dental residents share the opinion that many of these injuries are largely preventable. Time of admission to the emergency department was not explicitly reviewed for this data set, but the vast majority of e-scooter accidents occur in the evening and late night or early morning hours. It was not unexpected to find that 67% of patients reported alcohol use prior to their accidents. Additionally, when the decision to use e-scooters is made spontaneously, people rarely have helmets available, which almost certainly contributes to severity of injury. While people often ride e-scooters in pedestrian areas like sidewalks, paths, and crosswalks, people on e-scooters do not behave like pedestrians. Thus, drivers of vehicles are not accustomed to watching for and avoiding e-scooters. Many accidents involved riders losing control of the scooter, but a significant portion of the reported accidents were caused by riders being struck by vehicles, resulting in orthopedic, solid organ, and brain injuries in addition to facial and dental injuries.
Conclusion
This review sheds light on the potential life-changing consequences of riding e-scooters. We have selected three cases to highlight the severity of dental and facial trauma related to the use of e-scooters in the Denver metro area.
Case #1
This patient presented to the Denver Health Emergency Department after an e-scooter crash resulted in trauma to the middle and lower facial thirds. The patient was under the influence of alcohol the time of the accident. Injuries included left mandibular parasymphysis fractures; bilateral Lefort I fractures of the maxilla; right zygomaticomaxillary complex fractures; hard palate fracture; avulsed #7, #8, #23; displaced alveolar housing fracture involving #24-#26; traumatic impaction #22; root fracture #9; and multiple complex upper and lower lip lacerations (Figure 1a). He required admission to the OMS service and surgical intervention for his facial fractures. He was evaluated by GPR dental team and the teeth were all deemed non-restorable. He underwent ORIF of his facial fractures; extraction of non-restorable teeth #7, #8, #9, #22, #23, #24, #25, #26; and was placed into MMF with hybrid arch bars for stabilization of his palatal fractures (Figure 1b). His jaw was wired shut for two weeks. Dentoalveolar rehabilitation was discussed in the immediate postoperative phase of treatment. Unfortunately, the alveolar bone loss associated with his dental injuries was severe, and placement of future implants will require significant bone grafting to both the anterior maxilla and mandible. Due to extensive intraoral soft tissue injuries and healing surgical incisions, he was not an ideal candidate for ridge augmentation procedures at that time. At four weeks post injury, he had temporary dentures fabricated to restore his missing dentition. He was released from OMS recall three months post injury and will be an excellent candidate for ridge augmentation and implants in the future. Due to extensive alveolar bone loss, he will likely require autogenous bone grafting from the anterior iliac crest.

2a: 3-Dimensional reconstruction of CT facial bones showing facial fractures at time of presentation. 2b: Clinical photograph after placement of resin-bonded splint by GPR dental residents. 2c: Panorex radiograph obtained post-operatively showing reduction and fixation of facial fractures.
Case #2
The intoxicated patient presented to the emergency department after sustaining an e-scooter fall with direct chin strike resulting in a 3 cm submental laceration, lacerations to the right upper lip (2 cm and 1 cm), luxation of tooth #28 with Grade III mobility, Ellis class I fracture to #9, Ellis class II fracture to #8, and Ellis class III fracture to #12. The patient was also found to have a non-displaced fracture of the left mandibular angle and medially displaced left subcondylar fracture (Figure 2a). Lacerations were repaired in the emergency department by the OMS team and the GPR resident placed a resin bonded splint along with indirect pulp capping of teeth #8 and #12 in the emergency department (Figure 2b). At the initial visit, the patient complained of significant malocclusion and facial pain. The patient returned for outpatient surgical intervention five days later where she had ORIF of the left angle and closed reduction with MMF treatment for the left subcondylar fracture (Figure 2c). The patient remained on a no chew diet for six weeks and was released from fixation three weeks postoperatively. She was placed into guiding elastics for a total of six weeks postoperatively until the hybrid arch bars were removed. The patient had numerous restorative appointments including extractions of teeth #12 and #28 with implants placed at both sites. The mobility seen in teeth #8 and #9 had resolved by the third post-trauma month. At the completion of treatment, it was noted that the patient had a slight left posterior premature contact along with slight leftward deflection upon opening.
Case #3
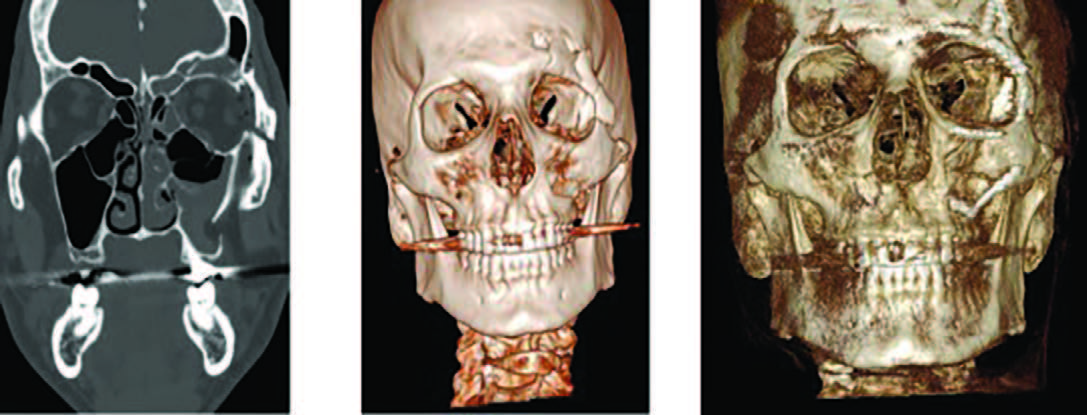
3a: Coronal slice of CT facial bones showing left side frontal bone and zygoma fractures at time of presentation. 3b: 3-Dimensional
reconstruction of CT facial bones showing facial fractures at time of presentation. 3c: 3-Dimensional reconstruction of CBCT obtained
post-operatively showing reduction and fixation of facial fractures.
The patient presented to the emergency department after sustaining an intoxicated e-scooter fall with a direct head strike and was found to have a 3 cm laceration to the left upper eyebrow, significantly depressed fracture of the left anterior table of the frontal sinus, fracture of the left superior orbital rim, displaced left zygomaticomaxillary complex fracture, and fractures of multiple walls of the left maxillary sinus (Figure 3a and 3b). The patient returned for outpatient surgery and underwent ORIF of the left frontal sinus, ORIF of the left superior orbital rim, and ORIF of the left zygomaticomaxillary complex (Figure 3c). The patient required overnight admission for postoperative monitoring and pain control. The patient returned for subsequent follow-up with no significant vision deficits, appropriate malar projection and no concern for ongoing/developing sinus pathology. The patient was noted to have left maxillary branch of the trigeminal nerve (CNV2) level A hypoesthesia that had not completely resolved at the last follow-up (three months postoperatively).
REFERENCES
Kahan R, Higinbotham S, Garoosi K, Lauder A. Electric Scooter-related Injuries Are Becoming More Frequent and Costly in Denver, CO. Clinical Orthopedics and Related Research. 2024 Aug 13. Online ahead of print.
Turner I, Shah M. Facial trauma due to e-scooters. British Dental Journal. 2023 January;234(2):74.
Sritharan R, Blore C, Arya R, McMillan K. E-scooter-related facial injuries: a one-year review following implementation of a citywide trial. British Dental Journal. 2023 January;234(2):102-105.
Grill FD, Roth C, Zyskowski M, Fichter A, Kollmuss M, Stimmer H, Deppe H, Wolff KD, Nieberler M. E-scooter-related craniomaxillofacial injuries compared with bicycle-related injuries – A retrospective study. Journal of Craniomaxillofacial Surgery. 2022 September;50(9):738-744.
McNulty M, Look N, Strage K, Lauder A. Orthopaedic Injuries After Introduction of Electric Scooters to Denver, Colorado. Journal of the American Academy of Orthopedic Surgery. 2022 September 15;30(18):897-902.
Authors
Boyd J Tomasetti D.M.D. – Dr. Tomasetti is a Board Certified Oral and Maxillofacial Surgeon and Attending at the Denver Health Oral and Maxillofacial Surgery Residency Program. He is a Past President of the AAOMS and CSOMS.
Jonathon Fergus D.D.S. – Dr. Fergus is a graduate of the University of Michigan School of Dentistry. He is a Third Year Resident at the Denver Health Oral and Maxillofacial Surgery Residency Program.
Akshay Shah D.D.S. – Dr. Shah is a graduate of the University of Colorado School of Dentistry. He is a Second Year Resident at the Denver Health Oral and Maxillofacial Surgery Residency Program.
Sara Anderson D.D.S., M.D. – Dr. Anderson is a Board Certified Oral and Maxillofacial Surgeon and the Program Director at the Denver Health Oral and Maxillofacial Surgery Residency Program. She is the Founder of Women in Oral and Maxillofacial Surgery Symposium.

