By Adam Evearitt, M.S., DABR
From the Summer 2016 Journal of the Colorado Dental Association
Dental x-rays have always given patients such a small amount of radiation that its effects are considered almost an afterthought. Dentists and hygienists are taught the details and intricacies of radiation dose and its interactions with the human body, but the public’s knowledge is limited. To make it understandable, in practice, dental staff members often compare dental radiation dose amounts to the amount of natural radiation a person gets from a few minutes in a plane or on the beach. But like a nagging little grain of sand in your shoe, this question of radiation can be frustrating because the general public has a fear of it. Questions from patients about the radiation emitted from dental x-ray machines come up on a regular basis, and some people even refuse exposure to the detriment of their own oral health.
Technology has changed a lot in the last few years, and these advances have had great benefits for what the dentist can now see with radiographic images. The change from film—the standard for decades in the field—to digital has had a great impact on the reduction of dose. This comes mainly from not having to repeat x-rays because digital receptors are much more forgiving, but also because there is a reduction in the amount of exposure needed to create an image. However, the advent of the Cone Beam CT volumetric imaging or 3-D technology—whatever it is called in your neck of the woods—has more than offset reductions in dose to the public from switching from film to digital imaging. Does this increase warrant concern from the radiation-frightened public?
First, let’s examine why dental x-rays have always been considered to be such a low amount. There is nothing magical about dental x-rays. They are the same sort of x-rays used in hospital imaging departments. Tooth is calcified structure, just like all the other bones in your body, so the amount and energies needed to penetrate that bone and make an image are the same. X-rays of teeth are actually very similar to finger or hand x-rays. The bone is about the same diameter, and the amount of soft tissue is also very similar. In fact, the technical aspects of imaging a finger and a tooth are just about the same. And similarly, the amount of radiation dose needed to penetrate the jaw and form an image for a panoramic x-ray is similar to the radiation needed for the elbow.
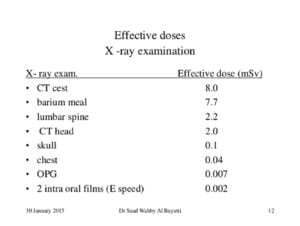
Figure 1.
So why do charts show the dose of dental x-rays as so much lower than “regular” x-rays? Reference Figure 1.
Notice that the dental exams are not compared to similarly sized medical exams. That might not be the point of this particular chart, but this chart with these exams is commonly used when comparing doses. Obviously much more x-ray radiation is needed to penetrate the skull or lower back than is needed to penetrate the teeth. But does that comparison make sense with the numbers on a purely size issue? In Figure 1, the dose from two intraoral films is 0.002 mSv. A lumbar spine is 2.2 mSv. That’s more than 1,000 times more radiation dose to the lower back than to the mouth. The biggest beer gut in the world isn’t 1,000 times the width of the cheek and gums. A difference between the width of a finger and the width of the abdomen for most people is only about 15 times.
The bigger difference between the lumbar spine exams and the intraoral exams is that the same amount of radiation to one area of the body can be more damaging than to another area of the body. This is because some tissue or organs are more radiosensitive than others. Physicists call this the tissue-weighting factor. For example, the ovaries—which would be in the x-ray field on many lower back exams—are much more prone to radiation damage than the skin in the cheek. Reference Figure 2 (below) for a chart listing the different weighting factors for organs in the human body.
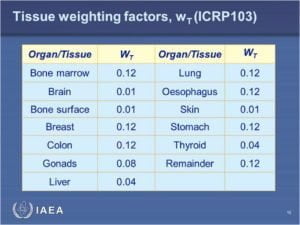
Figure 2.
The skin (cheek) and bone (teeth) have a 0.01 weighting factor and the gonads have a 0.08 weighting factor, which is eight times more. The colon has a weighting factor of 0.12, which is much larger than the skin and teeth as well. This is a bigger difference than just the difference in the change in thickness from the mouth to the abdomen.
Referring back to Figure 2, you see that the thyroid gland is listed as a 0.04 tissue weighting factor—five times that of the teeth and skin. During intraoral exams, the thyroid itself would not be included in the radiation field, but it does receive some scatter radiation that is generated in the patient as the x-rays scatter from the bone and some soft tissue. Even though this dose is extremely small, it is a concern that has received a lot of public attention, and the state of Colorado now requires dental offices to have thyroid shields along with the lead aprons.
The thyroid would not be included in any intraoral exams, but it is possible that it could be included in other exams like panoramic, cephlametric or 3D exams—especially in patients with unusual anatomy like kyphosis. Another radiosensitive organ not included in Figure 2 but still important to consider is the lens of the eye. Recently, the International Atomic Energy Association lowered its threshold for dose to the lens of the eye for occupational exposure to 20 mSv in a year averaged over five years with no single year exceeding 50 mSv. The public exposure remained unchanged from the last report, but it shows new evidence for cataracts showing up earlier than previously expected for radiation workers.
3-D Scans
The advent of volumetric imaging (3-D scanning) has changed everything when it comes to dose in dental imaging. As we saw from the previous discussion, the real reason that dose from dental x-rays was always considered so low that it was negligible is because the small fields of view and the low radiosensitivity of the bone and skin for intraoral exams. Dental 3-D scanners use fan beam technology and flat panel detectors, which is different than the technology used for CT scanners in a hospital. This provides some reduction in dose when compared to traditional CT machines, but many of the technical settings are the same. It’s hard to directly compare the dose of dental 3-D scanners to traditional hospital CAT scans because there is a lot going on behind the scenes.
The first thing to notice when looking at reported doses is that they do it in effective dose. This goes back to the tissue weighting factors. It is very important to know and teach the staff doing the exams that the low reported doses will change if there is positioning error or unusual patient anatomy, and unintended body parts show up in the scan. The manufacturers of dental 3-D scanners might take into account the salivary glands and other anatomy that is expected in the field of view, but the lens of the eye or thyroid is usually not expected.
The truth is there is nothing magical about the x-ray radiation used to create the great 3-D images in the new dental scanners. The detectors have improved greatly over the years, and they require less radiation than in the past to reconstruct those 3-D images. But the CT scanners in the hospitals do the same thing, and there is a certain minimum amount of energy that is required to go through the jaw no matter what scanner you are using.
Background Radiation
The most common way dentists explain the dose from their x-rays to concerned patients is to relate it to background radiation. If you just look at the numbers, you could say that one intraoral x-ray is equal to just 20 minutes of background radiation. While on the surface that might seem correct, it isn’t a direct comparison. One concentrated burst of x-ray radiation over a small area of the skin in one-tenth of a second is just not the same as the entire body getting bathed in a regular stream of radiation over 20 minutes. It might be technically the same amount of radiation when listed in a chart as dose, but it’s being applied to the body differently.
The same argument can be made for comparing risk of cancer formation. One website even lets you enter the effective dose equivalent of radiation you receive from a dental exam, and it will give you a number of your increased cancer risk from that exam. The data about cancer risk is based on the biological effect of ionizing radiation reports the government receives as they follow nuclear bomb survivors from Japan and other victims of radiation accidents over time. No one really knows if a single little burst of x-rays from dental exam can be extrapolated to a whole body dose that atomic bomb survivors received and then how their population showed an increased cancer risk decades later. Is it really scientifically valid to relate these two completely different events just because they have the same units of measure (dose)?
What is the truth that you can tell your patients?
- What we know is that radiation from dental exams has never been scientifically proven to raise the risk of cancer incidence.
- We know that the human body is used to getting bombarded with x-ray radiation from cosmic rays from space and radon gas in the air constantly from the moment we are conceived to the moment we die, so our bodies are used to repairing the damage caused by low amounts of radiation.
- We know that dental radiation has always been considered safer than other forms of medical radiation because it is directed to areas of the body that just aren’t radiosensitive. And if we shield the areas of concern—like the thyroid—and make sure that the lenses of the eyes and are kept out of the x-ray fields, then we are helping the patient to feel safe and protected.
About the Author: Adam Evearitt is the owner of Atom Physics and is a board certified medical physicist. He is also recognized by the state of Colorado as a qualified expert in x-ray machine inspection and shielding design. He has been working with medical radiation for the past 20 years.

