By Paul Bahn, D.M.D.
From the Spring 2023 Journal of the Colorado Dental Association
MIH (Molar Incisor Hypomineralization)
During my training, the term MIH or molar incisor hypomineralization, was not readily established and the understanding of the etiology was, and still to this day, not fully understood. With the appearance of a newly erupted first permanent molar that rapidly deteriorates, it is always a challenge from a short-term and long-term restorative perspective. MIH cases vary dramatically in their presentation and create challenges in managing timing of specific intervention, patient behavior and parental expectations.
Case Study
A 7-year-old male presented for a routine recall visit and extensive hypomineralization with secondary enamel breakdown noted on tooth #14 (Figure 1a). Radiographically the lesion was approximating the pulp and sensitivity to brushing and cold were frequent (Figure 1b). It is common in teeth that present with molar hypomineralization to have increased sensitivity and consequently poor oral hygiene, especially around the effected teeth. Pulpal vitality tests for immature pulp with an open apex are not reliable and clinical presentation and symptoms will often dictate how these teeth can be managed from a pulpal standpoint. In this particular instance, the gross hypomineralized and carious dentin was removed with a slow speed handpiece until more sound dentin was achieved. The goal was to obtain sound dentinal walls of the preparation and not to expose the pulp during excavation. Once a sound pulpal floor and clean axial walls were achieved an indirect pulp cap was placed using NuSmile NeoLINER™ LC and then restored with a glass ionomer (Figures 1c and 1d). The lesion presented here is fairly common within the scope of MIH.
At the CDA Annual Session in Snowmass Village, CO I will present a wide range of basic to complex lesions and scenarios related to the first permanent molars and the anterior incisors in the pediatric population that are hypomineralized.

Figure 1a: Initial clinical presentation of #14 with hypomineralized enamel and post-secondary breakdown.

Figure 1b: Initial radiographic presentation of #14.
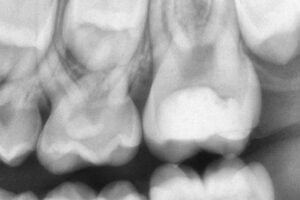
Figure 1c: Immediate post operative radiograph.

Figure 1d: Immediate post operative with glass ionomer restoration.
Laser Incorporation into Your Practice
The use of a carbon dioxide laser has a wide array of applications within the dental practice. The laser has advantages over the use of a surgical scissor or a scalpel by providing hemostasis and improving the visualization of the surgical field for a specific biopsy or lesion removal.
Case Study:
An 8-year-old female presented to our clinic with a dome shaped nodule in the area of the lower right lip (Figure 2a). The patient had a history of trauma but could not recall the specific time frame. The lesion was cyclic in nature and would expand, bleed and rupture and then fill back up with fluid. The lesion was painless but was negatively impacting speech and eating for the patient. Given the cyclic nature and issues related to lower lip function, the lesion was removed and sent for histological confirmation. The removal was performed under local anesthesia with the utilization of a carbon dioxide laser (Figure 2b). The wound area was fully cauterized during the excisional biopsy, allowing for full removal of the lesion. Upon completion of the biopsy, the wound site was reapproximated with two 3.0 chromic gut sutures that were buried into the excision site to eliminate the free ends of the sutures (Figure 2c). The utilization of the sutures enables primary closure of the wound site.
The biopsied sample was histologically confirmed to be a mucus extravasation phenomenon or more commonly a mucocele. This occurs due to the rupture of a minor salivary gland from sustained trauma. With the removal of the entire pathologic gland, the reoccurrence of this lesion will not occur, unless a secondary trauma occurs to an adjacent minor salivary gland.
The carbon dioxide laser can easily resolve a lesion like a mucocele, but that is only a small part of what it can achieve within the dental office.
At the CDA Annual Session in Snowmass Village, CO I will present more of the options that exist for the utilization and incorporation of a carbon dioxide laser into your practice.

Figure 2a: Initial presentation of dome shaped nodule in lower left lip.

Figure 2b: Immediate post excisional biopsy with a carbon dioxide laser

Figure 2c: Reapproximated margins of the excision site with two 3.0 chromic gut sutures.
Dr. Paul Bahn is the current program director for the Temple University Hospital-Northeastern Campus Pediatric Dental Resident Program. He currently serves as an Oral Board Examiner for the American Board of Pediatric Dentistry (ABPD) and is board certified by the ABPD and the American Board of Laser Surgery (ABLS).
|
Dr. Paul Bahn will be a featured CE speaker at the CDA Annual Session on Saturday, June 10 at the Viewline Resort Snowmass. Register for his courses and join your colleagues for a family-friendly weekend at the CDA Annual Session: cdaonline.org/annualsession |


